News
Stay informed about the latest developments in Gaza, the West Bank, including East Jerusalem, and Lebanon.
493 items found




Killed Saving Lives
25 November 2025




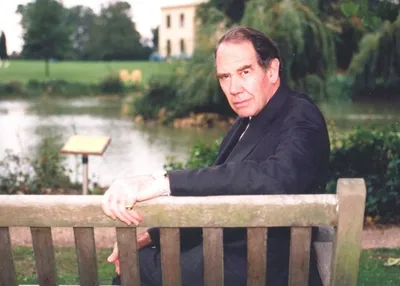
MAP appoints Steve Cutts as CEO
17 September 2025